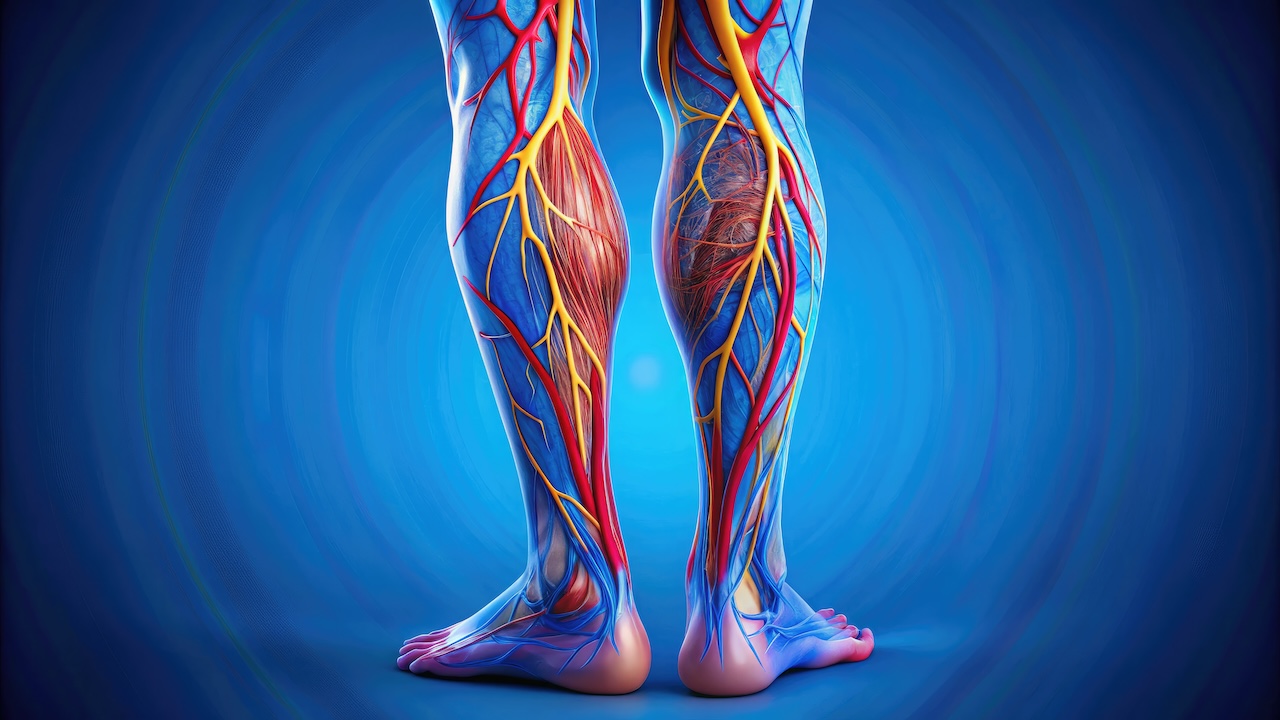
Venous leg ulcers frequently develop from chronic venous insufficiency. The following information gives a basic overview of how this health issue can lead to VLUs and how HBOT can be used to treat them.
What is Chronic Venous Insufficiency?
You can compare leg veins to a plumbing system. In this case, imagine the veins as pipes carrying blood to the heart. The veins’ tiny one-way valves serve as a miniature doorway when the legs are healthy. These doorways allow the blood to flow back up to the heart. Then, they close to prevent a backward flow of blood.
If you have chronic venous insufficiency, your valves begin to malfunction. In other words, those “little doors” have become damaged and do not close as they should. When this occurs:
- The flood that should flow toward the heart leaks backward and pools in the legs.
- The pooling builds pressure in the veins (like the water pressure building up in a clogged pipe).
- The increase in pressure causes fluids to leak from the veins and into the surrounding tissues.
Symptoms
This problem may cause:
- Swollen ankles or legs
- A heavy and tired feeling in the legs
- Changes in the skin – making the skin darker, itchy, or thicker
- Open sores, or venous leg ulcers, developing near the ankles
The problem can be likened to a traffic jam in the veins. The blood gets backed up instead of smoothly flowing upward as it should.
Risk Factors
People who increase their risk of venous insufficiency may:
- Be overweight
- Not getting enough exercise
- Stand or sit for long durations
- Be older
- Be pregnant
- Have a history of vein problems
Managing the Condition
Patients diagnosed with venous insufficiency may manage their condition by:
- Wearing compression stockings or socks that squeeze the legs in a way that promotes blood flow
- Walking regularly
- Elevating the legs above the heart when they rest
- Maintaining a healthy weight for their height
- Taking breaks and moving around if they sit or stand for a long time
Hyperbaric Oxygen Therapy (HBOT) and the Healing of VLUs
HBOT may also be beneficial in healing venous leg ulcers (VLUs), which often develop due to venous insufficiency.
Typically, oxygen travels through your bloodstream in two ways:
- Red blood cells carry most oxygen (97%), much like a bus carrying passengers.
- Blood plasma holds around 3% of oxygen.
Red blood cells or oxygen buses can’t reach the damaged tissue, as the blood vessels, like heavily traveled roads, become congested and, therefore, damaged. As a result, there’s not enough oxygen to promote healing.
HBOT Benefits
Hyperbaric Oxygen Therapy (HBOT) offers several notable benefits:
- It provides an oxygen-rich boost to your tissues, increasing their oxygen uptake beyond normal levels.
- HBOT helpts develop new blood vessels, like building new highways for oxygen and nutrient delivery.
- It reduces inflammation, like how ice reduces swelling after an injury.
- It fights bacteria that may be contributing to wound infections.
An Example of Current Research
Researchers have documented several cases where this therapy has been successful. For example, they reported a 65-year-old woman who had an ulcer for a year and a half. After 40 sessions of oxygen therapy, in addition to standard treatments, her ulcer healed almost completely.
Another study proved that the more time HBOT was applied (6 to 12 months), the more successful the outcome.
What Doctors Recommend for Wound Care
Typically, doctors recommend that patients spend about 90 minutes in the oxygen chamber five days a week for 6-8 weeks. Other therapies, such as compression bandages and HBOT, can also be used.
HBOT is Not for Everyone
While this treatment shows promise, it is not for everyone. Certain people with breathing conditions or those who are claustrophobic may not be able to opt for HBOT. The cost can also be prohibitive, though researchers believe HBOT may save money by accelerating wound healing.
Inside the HBOT Chamber
Within this HBOT chamber (which can be compared to a submarine), two things happen:
- Pressure increases (like being underwater).
- You breathe 100% pure oxygen (compared to the usual 21% in normal air).
The combination of increased pressure and pure oxygen is essential. Think of the process of carbonating a drink. Pressure can dissolve more gas into the liquid. Similarly, under hyperbaric conditions, oxygen can dissolve into your blood plasma at levels up to 20 times greater than usual!
This oxygen-rich plasma can penetrate even the smallest damaged vessels, reaching injured tissues that normal blood flow may not be able to get. It’s like deploying a fleet of tiny delivery drones that can reach areas where regular delivery trucks (red blood cells) cannot navigate.
Why HBOT Works
The oxygen triggers a healing response:
- HBOT creates new blood vessels (imagine your body constructing new roads to alleviate traffic jams).
- It activates specialized cells called stem cells, which are vital for repair.
- It helps your body fight infection.
- It reduces harmful inflammation that can slow healing.
Now that you know how this treatment works, you can see why it may be effective even when other treatments have failed.
Benefits of HBOT for Wound Healing
The benefits of HBOT for wound healing are multifaceted:
- Enhanced Oxygen Delivery: HBOT increases tissue oxygen levels far beyond what can be achieved with normal breathing, even in areas with compromised blood flow.
- Stimulation of Angiogenesis: The increased oxygen levels help grow blood vessels and improve blood flow to an affected site.
- Stem Cell Activation: HBOT activates stem cells, which support tissue repair and regeneration.
- Anti-Inflammatory Effects: HBOT helps to reduce inflammation, which can hinder the healing process.
- Antibacterial Action: HBOT can help fight bacteria, reducing infection risk and reducing healing times..
Key Takeaways
- Oxygen is essential for tissue healing. Under normal circumstances, red blood cells and blood plasma transport oxygen throughout the body.
- Packed with hemoglobin, red blood cells carry the most oxygen (approximately 97%), while a smaller portion (around 3%) is dissolved directly in the blood plasma.
- In venous leg ulcers, the damaged blood vessels and surrounding tissue create a low-oxygen environment.
- This oxygen deficit impairs the body’s ability to heal the wound, making VLUs chronic and challenging to treat.
- Hyperbaric Oxygen Therapy (HBOT) offers a solution by increasing the amount of oxygen dissolved in the blood plasma.
- The therapy involves lying in a pressurized chamber and receiving 100% pure oxygen.
- Again, the increased pressure and pure oxygen environment allow the blood plasma to absorb significantly more oxygen than usual.
References/Case Studies
1.Losev RZ, Burov IA, Mikul’skaia IG, Iakusheva IA. Evaluation of microcirculation in elderly patients with venous trophic ulcers. Angiol Sosud Khir. 2005;11:65-72. doi:2005/07/22. [PubMed] [Google Scholar]
2. Abbade LPF, Lastória S. Venous ulcer: epidemiology, physiopathology, diagnosis and treatment. Int J Dermatol. 2005;44:449-456. doi: 10.1111/j.1365-4632.2004.02456.x. 2005/06/09. [DOI] [PubMed] [Google Scholar]
3.Milovanova TN, Bhopale VM, Sorokina EM, et al. Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo. J Appl Physiol (1985) 2009;106:711-728. 2008/11/22. doi: 10.1152/japplphysiol.91054.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
4.Thom SR, Bhopale VM, Velazquez OC, Goldstein LJ, Thom LH, Buerk DG. Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol. 2006;290:H1378-H1386. doi: 10.1152/ajpheart.00888.2005. 2005/11/22. [DOI] [PubMed] [Google Scholar