Hyperbaric oxygen therapy (HBOT) allows patients to breathe pure oxygen inside a chamber – where the pressure is bumped up well above normal. In simple terms, this extra pressure lets oxygen seep more thoroughly into the blood plasma—not just hitching a ride on red blood cells but dissolving into the fluid part of the blood.
This process can kick-start healing, ease inflammation, and sometimes even boost the effectiveness of certain medicines. In urological oncology, doctors have increasingly started to see HBOT as a handy extra tool for handling complications and helping patients recover more fully. This post goes into the nuts and bolts of how HBOT functions, its possible roles, and a few case examples that bring the idea into sharper focus.
Understanding Hyperbaric Oxygen Therapy
When one steps into a pressurized chamber, the partial pressure of oxygen in the body’s tissues climbs noticeably. Usually, hemoglobin ferries oxygen around, but under these conditions, more oxygen dissolves into the blood plasma, sometimes described as hyperoxygenation.
Generally speaking, this extra boost can encourage tissue repair, tone down inflammation, and even enhance the benefits of medications. It’s a fascinating interplay between physical pressure and biological response, like nature’s way of rebalancing itself, albeit with a technical twist.
Physiological Effects of HBOT
There are several bodily reactions that HBOT sets off that seem especially pertinent in the realm of urology oncology:
• Angiogenesis – new blood vessel growth seems to be stimulated, which helps reestablish blood flow to tissues that have been damaged.
• Wound Healing – higher oxygen levels help drive collagen production and speed up the closing process of wounds.
• Anti-inflammatory Effects – by tweaking the behavior of inflammatory cells and their by-products, HBOT can calm inflammation.
• Antimicrobial Effects—The abundance of oxygen makes it harder for certain bacteria to thrive (and can even give antibiotics a bit of extra push).
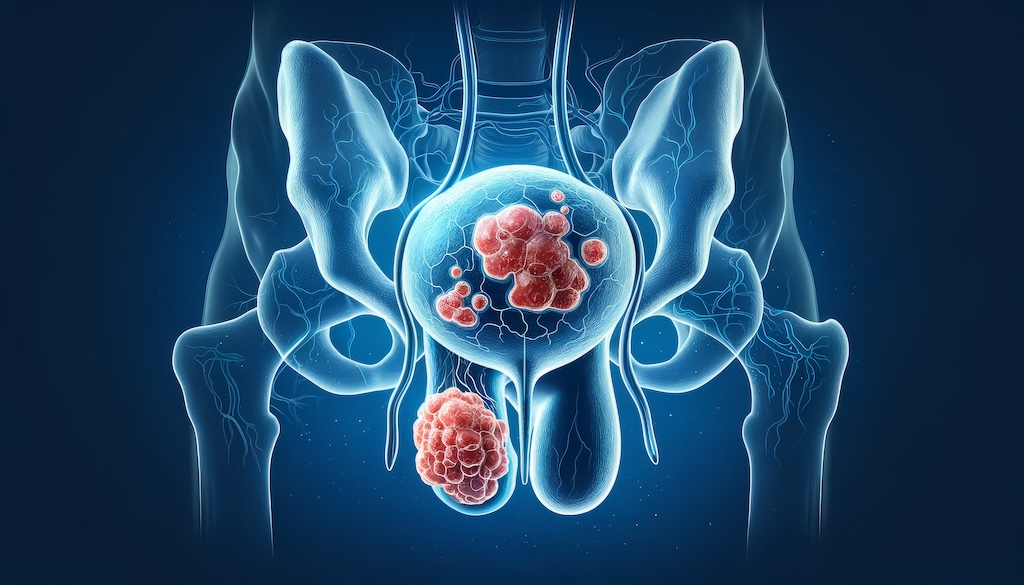
Applications in Urology Oncology
In practice, HBOT is used in urological oncology not as a first-line treatment but as an adjunct to tackle some stubborn complications—often following radiation therapy or surgery. For example, radiation for pelvic cancers (like those of the prostate or bladder) can sometimes cause what’s known as radiation-induced cystitis (RIC).
This condition often leaves the bladder lining inflamed and damaged, leading to symptoms such as blood in the urine, frequent trips to the bathroom, and discomfort. HBOT has shown promise in gently nudging tissue repair and dialing back inflammation in these cases.
Another urological-related condition is osteoradionecrosis (ORN) of the pelvis. Here, the bone essentially starts to die after radiation, which severely hampers the body’s natural repair mechanisms. ORN can pop up in patients treated for either gynecologic or urological cancers. Generally speaking, HBOT may help enhance healing and slow down by improving oxygen flow to the affected bone. There are also can.
There are also cases where wound healing after surgery doesn’t quite go as planned, especially in those who’ve had previous radiation. With HBOT coming into play, increased oxygen delivery can jump-start tissue regeneration and help mend more quickly and at a better pace.
Case Studies – Examples of the Healing Power of HBOT
One illustrative instance involved a 65-year-old gentleman with a history of prostate cancer. After receiving external beam radiation therapy, he began suffering from ongoing hematuria (blood in the urine) and a constant need to void.
A cystoscopy revealed widespread telangiectasias and a fragile bladder l screamed radiation-induced cystitis. He then underwent 30 HBOT sessions at roughly 2.4 ATA for 90 minutes each. Strangely enough, his bleeding stopped, ed and his bathroom trips normalized; a follow-up later showed an apparent, marked reduction in the bladder’s abnormal appearance.
In another case, a 72-year-old woman, previously treated for cervical cancer with radiation, developed piercing pelvic pain and non-healing ulcers in her perineal region. Imaging indicated osteoradionecrosis. Throughout 40 HBOT sessions (each lasting about 120 minutes at 2.0 ATA), her pelvic pain gradually lessened, the ulcers started to heal, and subsequent imaging even hinted at some new bone growth—a hopeful sign indeed.
A third example features a 58-year-old male who underwent a radical cystectomy for bladder cancer. Post-surgery, he encountered delayed wound healing—a complication not uncommon after such invasive procedures, particularly if prior radiation has been a factor. With HBOT added to his recovery plan, his wound slowly began to improve, showcasing how increased oxygenation can help steer the healing process back on track—even if progress sometimes looks uneven.
Overall, HBOT’s role in urology oncology seems to emerge as a promising strategy, with its effects on tissue oxygenation leading to benefits from enhanced wound repair to diminished inflammation. In many cases, it offers an alternative route for recovery when standard treatments run into complications, making it a fascinating area for ongoing study and application.
Using HBOT in Urology Practices
Urologists carefully examine the patient’s history, the exact problem, and any possible contraindications for urology conditions before considering HBOT. Generally speaking, teaming up with a well-regarded hyperbaric oxygen center and a crew of experienced physicians is essential. Patient selection and treatment setup should all be tailored individually to get the best results while keeping risks low.
Side Effects
Even though hyperbaric oxygen therapy is safe, there are still a few possible side effects. For example, patients might experience ear and sinus pressure issues, rarely seen oxygen toxicity, bouts of claustrophobia, or even some temporary vision changes.
Future Research
Looking ahead, research on HBOT in urology oncology is ongoing. Re-studies may uncover new ways to apply the therapy, refine the treatment routines, or even combine it with other therapies. More investigation is needed to understand how HBOT works fully and its long-term impact on urological conditions.
In conclusion, hyperbaric oxygen therapy is a promising additional tool for addressing complications in urology oncology. Its knack for boosting tissue oxygen levels, supporting wound healing, and cutting down inflammation can be handy when dealing with radiation-induced injuries and surgical complications. Urology oncologists should consider the benefits and limitations of HBOT and consider it part of a broader, comprehensive care plan.
_________________________________________________________
References:
(1) Kaufman DS, Zietman AL, Dahl DM, Harisinghani MG, Wu CL. Case records of the Massachusetts General Hospital. Case 5-2011. A 65-year-old man with hematuria after prostate cancer treatment. N Engl J Med. 2011 Feb 17;364(7):667-75. doi: 10.1056/NEJMcpc1005310. PMID: 21323545.
(2) Feltl D, Vosmik M, Jirásek M, Stáhalová V, Kubes J. Symptomatic osteoradionecrosis of pelvic bones in patients with gynecological malignancies-result of a long-term follow-up. Int J Gynecol Cancer. 2006 Mar-Apr;16(2):478-83. doi: 10.1111/j.1525-1438.2006.00540.x. PMID: 16681714.
(3) Nasrallah AA, Mansour M, Abou Heidar NF, Ayoub C, Najdi JA, Tamim H, El Hajj A. Risk factors for wound dehiscence following radical cystectomy: a prediction model. Ther Adv Urol. 2021 Dec 5;13:17562872211060570Doioi: 10.1177/17562872211060570. PMID: 35173813; PMCID: PMC8842309.